Pearl is a clinical professor of plastic surgery at the Stanford University School of Medicine and is on the faculty of the Stanford Graduate School of Business. He is a former CEO of The Permanente Medical Group.
Five years ago, with the 2018 midterm elections fast approaching, voters pegged healthcare as their No. 1 election issue.
Since that time, the U.S. healthcare system has fallen further behind its global peers, notching far more failures than wins.
Looking back, the rate of chronic disease has climbed while life expectancy has fallen. Nearly half of American adults now struggle to afford healthcare as a growing mental-health crisis grips our country. Maternal mortality is on the rise while healthcare disparities continue expanding along racial and socioeconomic lines.
The Biden administration, for its part, aims to remedy these failings by making healthcare (and healthcare costs, in particular) a signature issue of the president’s reelection bid. But beyond efforts to lower drug prices, there’s not much in the political pipeline to suggest the next five years of healthcare will be better than the last five.
What we need are practicable, cost-effective measures that elected officials and medical leaders can implement relatively quickly. Here are three actions that would reshape American medicine and improve our nation’s health:
Shore Up Primary Care
The world’s most-effective and highest-performing healthcare systems deliver better quality of care at significantly lower costs than in the United States. One major difference: primary care.
In most high-income nations, primary care makes up roughly half of the physician workforce. In the United States, it accounts for less than 30% —with a projected shortage of 48,000 primary care physicians by 2034.
More than any other specialty, primary care improves life expectancy while lowering overall medical expenses. It happens by (a) screening for and preventing diseases and (b) helping patients with chronic illness avoid the deadliest, costliest complications (heart attack, stroke, cancer).
However, it takes three years after medical school to train a primary care physician. So, to reverse the deficit, the government must act immediately.
First, Congress would earmark an additional $200 million toward annual resident education funding. The money would create 1,000 more primary-care residency positions each year (at less than 0.2% of total federal spending on medical care).
Then, to attract the best medical students to primary care, the Centers for Medicare & Medicaid Services (CMS) would shift reimbursement rates, narrowing the $108,000 pay gap between primary care and specialist physicians.
These actions would shore up primary care and bolster the health of millions.
Use Technology To Expand Access
Thirty million Americans live without health insurance. Tens of millions more are underinsured.
To make matters worse, national medical expenditures are projected to rise from $4.3 trillion to $7.2 trillion over the next eight years. The Medicare trust fund will become insolvent years earlier. Healthcare is rapidly becoming unaffordable and inaccessible for most Americans.
Most industries that have overcome similar financial headwinds relied on technology as a solution. Healthcare can take a page from this playbook by expanding the use of telemedicine and generative AI.
During the pandemic, telehealth enabled convenient, cost-effective, high-quality medical care. Virtual visits accounted for 69% of all physician appointments. However, its use is now plummeting as states reinstitute outdated restrictions, prohibiting doctors from providing telemedical care to patients in neighboring states.
It’s illogical that a patient can drive across state lines for care but can’t get the same expertise virtually and more affordably from home. Legislators need to loosen these restrictions to facilitate greater access for patients with both physical and mental-health problems.
Likewise, the “hospital at home” approach emerged during the pandemic as physicians faced a shortage of beds. As with telemedicine, patients and clinicians praised the quality and convenience of home-based care.
Building on that success, doctors can now effectively monitor the clinical progress of patients 24/7, at home, by combining wearable devices with generative AI tools like ChatGPT.
To encourage broad implementation, the Federal Drug Administration and National Institute of Health should support pilot projects. And rather than restricting powerful and inexpensive technologies like generative AI, regulators should spur and facilitate their use.
Reduce Disparities In Medical Care
American healthcare is a system of haves and have-nots, where income and race heavily determine the quality of care patients receive.
Black patients, in particular, experience poorer medical outcomes and greater difficulty accessing state-of-the-art treatments. In childbirth, Black mothers die at twice the rate of white women, even when data are corrected for insurance and financial status.
Generative AI applications like ChatGPT can help, provided that clinicians use them to provide more inclusive, equitable care. Whereas researchers designed past AI tools to replicate how doctors practice—consequently including human bias in the data—today’s technologies can detect and even prevent prejudicial care.
To accomplish this, hospital leaders would connect electronic health record (EHR) systems with next-gen AI. With the right prompts, these systems would notify clinicians when they’re providing inferior medical treatment to patients of different racial or socioeconomic backgrounds. To support the effort, CMS would provide financial incentives to hospitals that use this technology for greater equality.
Bringing bias to consciousness will help reverse our nation’s embarrassingly high maternal mortality rate.
We can stop the slide of American healthcare over the next five years, but only by acting now. I urge medical leaders and elected officials to join forces and implement these highly effective, inexpensive approaches to rebuilding primary care, lowering medical costs, improving access and making medical practice more equitable. There’s no more time to waste.

















 A woman prepares to cast her vote on May 4, 2025 in Bucharest, Romania. The first round of voting begins in the re-run of Romania's presidential election after six months since the original ballot was cancelled due to evidence of Russian influence on the outcome. Then far-right candidate Calin Georgescu surged from less than 5% days before the vote to finish first on 23% despite declaring zero campaign spending. He was subsequently banned from standing in the re-rerun, replaced this time round by George Simion who claims to be a natural ally of Donald Trump.Getty Images, Andrei Pungovschi
A woman prepares to cast her vote on May 4, 2025 in Bucharest, Romania. The first round of voting begins in the re-run of Romania's presidential election after six months since the original ballot was cancelled due to evidence of Russian influence on the outcome. Then far-right candidate Calin Georgescu surged from less than 5% days before the vote to finish first on 23% despite declaring zero campaign spending. He was subsequently banned from standing in the re-rerun, replaced this time round by George Simion who claims to be a natural ally of Donald Trump.Getty Images, Andrei Pungovschi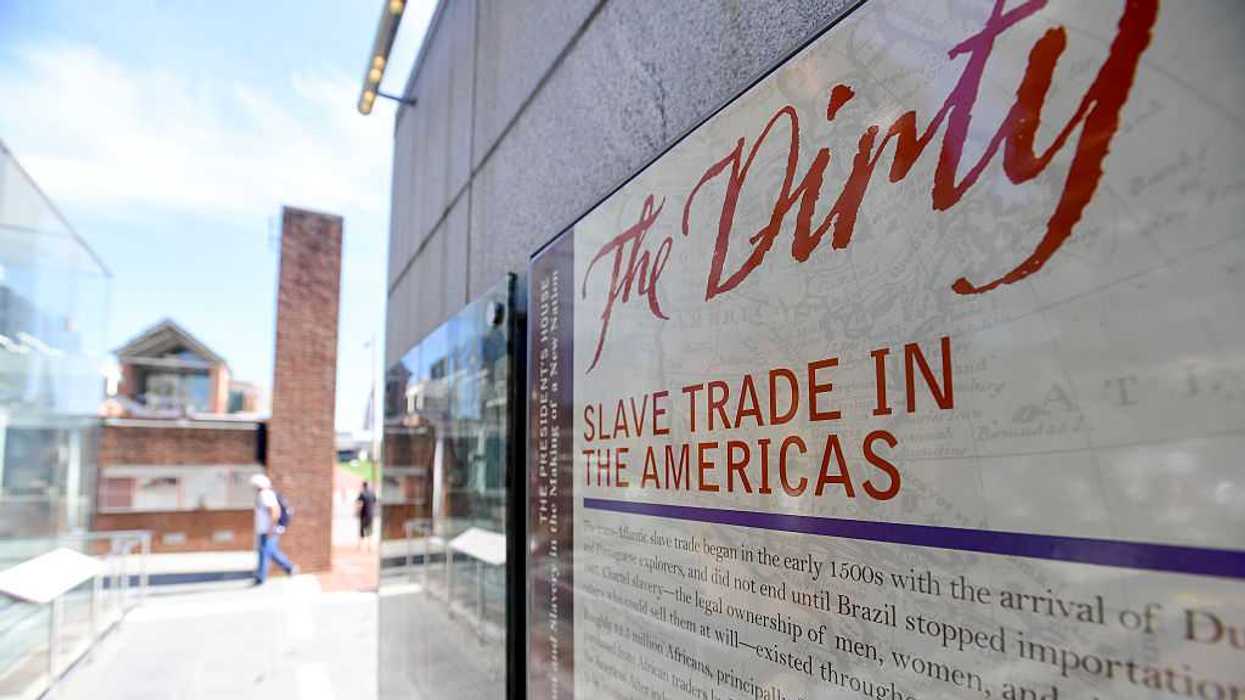
Trump & Hegseth gave Mark Kelly a huge 2028 gift