Pearl is a clinical professor of plastic surgery at the Stanford University School of Medicine and is on the faculty of the Stanford Graduate School of Business. He is a former CEO of The Permanente Medical Group.
This is the first entry in a two-part op-ed series on institutional racism in American medicine.
The story of American medicine is one of incredible scientific advancements, from the use of penicillin to treat syphilis and other bacterial infections to the countless biomedical breakthroughs made possible by cell-line research.
Too often, however, these stories ignore an uncomfortable truth: Some of our nation's most significant medical discoveries were made possible through the mistreatment of Black patients — from the exploitation of African American farmers during the Tuskegee syphilis experiments to the tragic case of Henrietta Lacks, a Black patient whose cells were stolen by doctors and used for decades of cell-line research.
Racism is woven into our nation's medical past but is also part of our present, as evidenced by the Covid-19 crisis. From testing to treatment, Black and Latino patients have received a lower quality and quantity of care compared white Americans.
The biases of individual doctors and researchers aren't always the biggest barriers to equitable health care. Often, the problem is institutional.
Institutional (or systemic) racism is invisible yet omnipresent. It is woven into the fabric of American health care, embedded into the practices, policies and perceptions of the entire industry.
At some point during medical school, all future doctors are instructed to treat everyone equally, regardless of a person's race, ethnicity, gender, religion or sexual orientation. Studies have shown just how difficult this edict proves in practice.
Even when physicians have the best of intentions, their actions are beset by unconscious prejudices. Researchers have found that two out of three clinicians harbor what is called an "implicit bias" against African Americans and Latinos. These are biases that exist outside the doctor's awareness but are nonetheless harmful to minority patients.
In one example, epidemiological data demonstrate that Black individuals have experienced a two to three times higher likelihood of dying from Covid-19 than white patients.
Physicians attribute this discrepancy to the "social determinants of health," a phrase that encapsulates the many aspects of life that influence our health, including where we live, work, play and socialize. But before we accept this explanation and let health care professionals off the hook, consider what we learned early in the pandemic: According to national studies, white patients who came to the emergency room with symptoms likely to be Covid-19 were tested far more often than Black patients with identical symptoms.
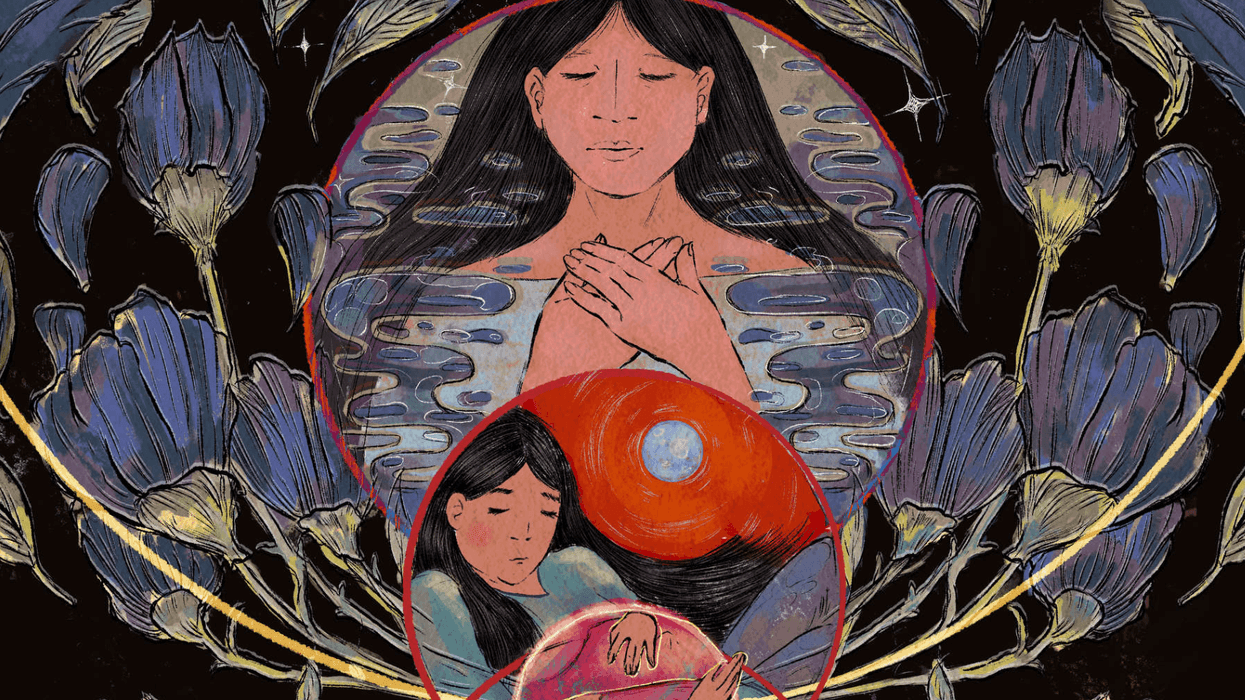
A distressing example of institutional racism involves childbirth. Most Americans don't realize it, but the United States ranks last among all developed nations in maternal mortality (the measure of how often mothers die during or soon after childbirth).
Most of these deaths could be prevented, and yet the maternal mortality rate has been increasing in the United States since 2000. Two decades after The Journal of Perinatal Education first described the issue of racial disparities in maternal care as "alarming," Black women remain three times more likely to die from childbirth than white women.
Obstetricians know the most common causes of maternal death are (a) unrecognized bleeding and (b) uncontrolled high blood pressure. What they can't explain is exactly why a woman's skin color has such a significant influence on her risk of dying. Ask doctors what's going on and they'll list a number of contributing factors, ranging from the higher risk of hypertension in Black patients to greater life stresses to differences in diet and education.
But none of those factors help explain this: When the treating clinician is Black, the disparity in deaths between white and Black mothers all but vanishes.
The problem in understanding this discrepancy isn't a lack of data. Almost all U.S. hospitals have comprehensive inpatient electronic health records that provide a rich tapestry of details about the women giving birth and the care they receive. And as of 2017, all 50 states were required to add a standardized "maternal mortality checkbox" to their data reporting systems.
And yet we still don't know why the race of the doctor makes such a difference or how to close the gap when the physician is white. We also don't know if the race of the nurses providing the care matters. We also don't know whether the frequency of blood-pressure monitoring or care checks varies based on the patient's race, the staff member's race or both.
Most medical research focuses on the causations or correlations between two easily isolated data sets (like the race of doctors and the mortality of patients). Addressing systemic racism in medicine requires that we analyze far more data (all at once) than we do today.
In my next writing, I will explore how artificial intelligence might be the perfect application for this task but also how predictive health care algorithms used in AI can, themselves, have design flaws that result in unintended discriminatory biases.















Eric Trump, the newly appointed ALT5 board director of World Liberty Financial, walks outside of the NASDAQ in Times Square as they mark the $1.5- billion partnership between World Liberty Financial and ALT5 Sigma with the ringing of the NASDAQ opening bell, on Aug. 13, 2025, in New York City.
Why does the Trump family always get a pass?
Deputy Attorney General Todd Blanche joined ABC’s “This Week” on Sunday to defend or explain a lot of controversies for the Trump administration: the Epstein files release, the events in Minneapolis, etc. He was also asked about possible conflicts of interest between President Trump’s family business and his job. Specifically, Blanche was asked about a very sketchy deal Trump’s son Eric signed with the UAE’s national security adviser, Sheikh Tahnoon.
Shortly before Trump was inaugurated in early 2025, Tahnoon invested $500 million in the Trump-owned World Liberty, a then newly launched cryptocurrency outfit. A few months later, UAE was granted permission to purchase sensitive American AI chips. According to the Wall Street Journal, which broke the story, “the deal marks something unprecedented in American politics: a foreign government official taking a major ownership stake in an incoming U.S. president’s company.”
“How do you respond to those who say this is a serious conflict of interest?” ABC host George Stephanopoulos asked.
“I love it when these papers talk about something being unprecedented or never happening before,” Blanche replied, “as if the Biden family and the Biden administration didn’t do exactly the same thing, and they were just in office.”
Blanche went on to boast about how the president is utterly transparent regarding his questionable business practices: “I don’t have a comment on it beyond Trump has been completely transparent when his family travels for business reasons. They don’t do so in secret. We don’t learn about it when we find a laptop a few years later. We learn about it when it’s happening.”
Sadly, Stephanopoulos didn’t offer the obvious response, which may have gone something like this: “OK, but the president and countless leading Republicans insisted that President Biden was the head of what they dubbed ‘the Biden Crime family’ and insisted his business dealings were corrupt, and indeed that his corruption merited impeachment. So how is being ‘transparent’ about similar corruption a defense?”
Now, I should be clear that I do think the Biden family’s business dealings were corrupt, whether or not laws were broken. Others disagree. I also think Trump’s business dealings appear to be worse in many ways than even what Biden was alleged to have done. But none of that is relevant. The standard set by Trump and Republicans is the relevant political standard, and by the deputy attorney general’s own account, the Trump administration is doing “exactly the same thing,” just more openly.
Since when is being more transparent about wrongdoing a defense? Try telling a cop or judge, “Yes, I robbed that bank. I’ve been completely transparent about that. So, what’s the big deal?”
This is just a small example of the broader dysfunction in the way we talk about politics.
Americans have a special hatred for hypocrisy. I think it goes back to the founding era. As Alexis de Tocqueville observed in “Democracy In America,” the old world had a different way of dealing with the moral shortcomings of leaders. Rank had its privileges. Nobles, never mind kings, were entitled to behave in ways that were forbidden to the little people.
In America, titles of nobility were banned in the Constitution and in our democratic culture. In a society built on notions of equality (the obvious exceptions of Black people, women, Native Americans notwithstanding) no one has access to special carve-outs or exemptions as to what is right and wrong. Claiming them, particularly in secret, feels like a betrayal against the whole idea of equality.
The problem in the modern era is that elites — of all ideological stripes — have violated that bargain. The result isn’t that we’ve abandoned any notion of right and wrong. Instead, by elevating hypocrisy to the greatest of sins, we end up weaponizing the principles, using them as a cudgel against the other side but not against our own.
Pick an issue: violent rhetoric by politicians, sexual misconduct, corruption and so on. With every revelation, almost immediately the debate becomes a riot of whataboutism. Team A says that Team B has no right to criticize because they did the same thing. Team B points out that Team A has switched positions. Everyone has a point. And everyone is missing the point.
Sure, hypocrisy is a moral failing, and partisan inconsistency is an intellectual one. But neither changes the objective facts. This is something you’re supposed to learn as a child: It doesn’t matter what everyone else is doing or saying, wrong is wrong. It’s also something lawyers like Mr. Blanche are supposed to know. Telling a judge that the hypocrisy of the prosecutor — or your client’s transparency — means your client did nothing wrong would earn you nothing but a laugh.
Jonah Goldberg is editor-in-chief of The Dispatch and the host of The Remnant podcast. His Twitter handle is @JonahDispatch.