Current Issue
In the coming year, millions of Americans could see their health insurance premiums rise, or lose coverage entirely, as key federal supports for affordable care are set to expire. The American Rescue Plan Act of 2021 (ARPA) subsidies under the Affordable Care Act (ACA) marketplace, which were later extended by the Inflation Reduction Act, are scheduled to expire at the end of 2025. According to one analysis, if these enhanced subsidies expire, premiums on average could increase by 25-100 percent. At the same time, several states are reducing Medicaid rolls following the end of the pandemic-era continuous coverage requirement. Over 25 million people had been disenrolled from Medicaid and CHIP during this process in 2024. Together, these changes could redefine U.S. healthcare access, reigniting debates about public health and fiscal restraint.
Background
The ACA, passed in 2010, aimed to make health insurance more accessible for millions of uninsured Americans by expanding Medicaid eligibility and creating subsidized plans under the premium tax credit. The ARPA of 2021 significantly increased those marketplace subsidies, eliminating the 400% of poverty threshold for eligibility and reducing the percentage of income that enrollees must pay in premiums. As a result, the number of people eligible for marketplace subsidies increased from 18.1 million to 21.8 million from 2020-2021. Meanwhile, pandemic policies prevented states from disenrolling almost all Medicaid and CHIP enrollees for over three years. When this continuous coverage requirement ended in April of 2023, states began to reevaluate the eligibility of tens of millions of people. The expiration of ARPA temporary subsidies combined with the end of continuous Medicaid coverage set the stage for a contentious healthcare market next year.
Arguments for and Against Medicaid Cuts
Supporters of allowing the subsidies to expire and tightening Medicaid eligibility argue that these measures are necessary to reduce federal spending and restore fiscal discipline. For example, one analyst reported that ACA-related premium tax credits and related spending accounted for about 6% of federal healthcare spending in 2023, and projections show it shrinking further. Fiscal conservatives argue that the temporary nature of the pandemic-era expansions was clear from the start, and that continuing them indefinitely would distort the original design of the ACA and burden taxpayers.
Opponents of the cuts, however, warn that cutting back subsidies and shrinking Medicaid benefits would reverse more than a decade of progress in reducing the rate of uninsurance. One article estimates that 4-5 million additional Americans could become uninsured. Additionally, disenrollment data shows that procedural and administrative barriers have already contributed to millions of terminations in Medicaid, even where people may still be eligible. These critics argue that healthcare coverage is a public good, and that covering more people reduces uncompensated care costs for hospitals, improves population health outcomes, and increases economic stability for families.
Political and Public Health Implications
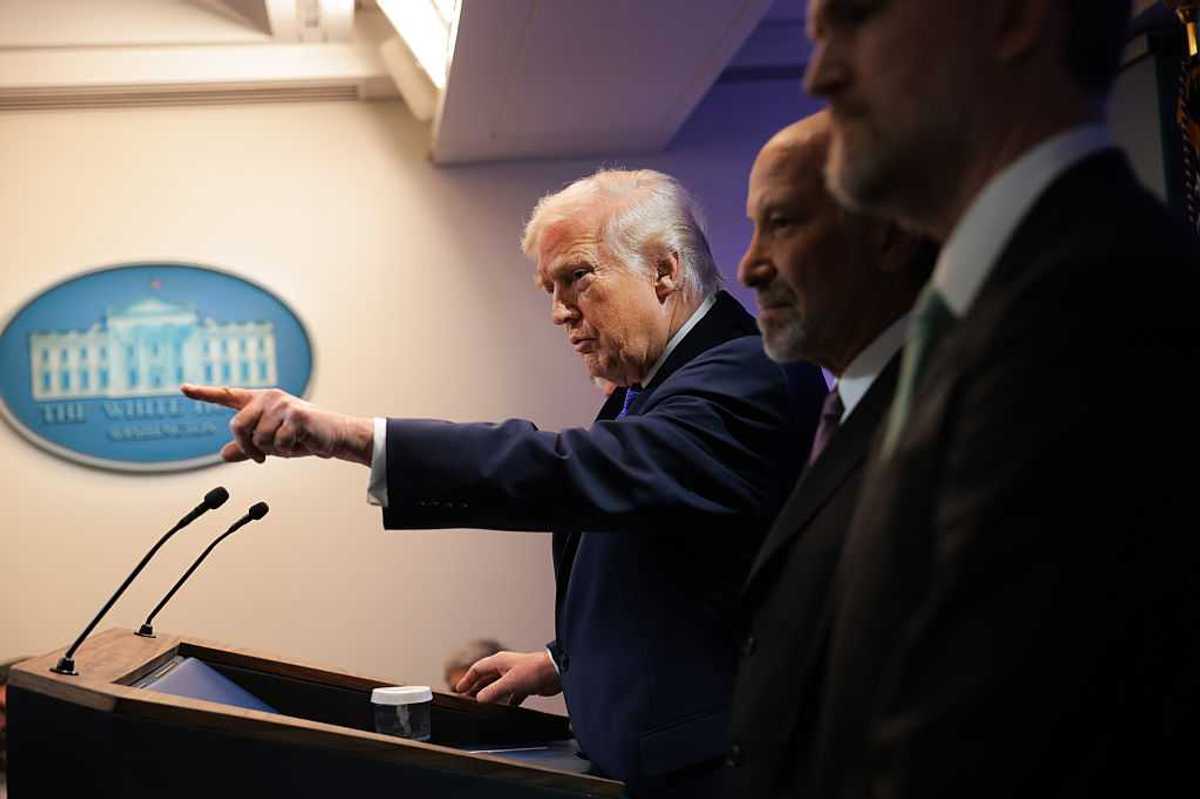
The debate over healthcare subsidies and Medicaid reflects a broader ideological divide in Washington. For the most part,Democrats favor extending or making the enhanced subsidies permanent, while Republicans emphasize deficit reduction and returning to pre-pandemic policy norms. This issue has become a key point of focus during the government shutdown.
From a public health perspective, the health outcomes related to this situation are equally important. If subsidies lapse and Medicaid cuts continue, the uninsured rate will likely rise, threatening preventative care, maternal health, and chronic disease management. Hospitals in rural and underserved areas which are already operating under thin margins could face higher uncompensated care burdens, potentially forcing reduction in services or closures. This is especially important as underserved communities and those of color who have already seen disparate impacts during the pandemic may be more vulnerable to coverage loss.
Conclusion
As the 2025 expiration date approaches, lawmakers must make a choice: whether to extend federal assistance and maintain current levels of coverage, or allow the system to contract in the name of fiscal prudence. This decision will shape the affordability of healthcare for millions. Whether Congress chooses to sustain or scale back these programs, one thing is clear: the future of U.S. healthcare once again hangs in the balance.
How Expiring Subsidies and Medicaid Cuts Could Reshape U.S. Access to Care was originally published by the Alliance for Civic Engagement and is republished with permission.















 Native American women face higher rates of death than other demographics. (Oona Zenda/KFF Health News)
Native American women face higher rates of death than other demographics. (Oona Zenda/KFF Health News)

Trump & Hegseth gave Mark Kelly a huge 2028 gift